No content results match your keyword.
Content
You have successfully logged out.
Ultrasound Guided IV Placement
Ultrasound guidance provides additional visibility to healthcare works when inserting a peripheral IV catheter compared to the conventional technique of seeing and palpating the vein.

Ultrasound-guided peripheral IV insertions have been shown to improve overall success rates up to 90% for patients with difficult intravenous access (DIVA), while using conventional techniques for peripheral IV insertions on DIVA patients only has a success rate of 25-30%1. This means it is highly likely that a DIVA patient will be stuck twice before the completion of their infusion therapy. Often times when a patient has experienced multiple failed peripheral IV insertion attempts, they are escalated to more costly, invasive and risky devices such as central lines.2 Therefore introducing ultrasound guidance as added vein visualization for DIVA patients could increase first stick success and improve patient outcomes.3
Patients with difficult IV access are frequently subjected to repeated attempts of vascular access by multiple practitioners.4 This can lead to progressive vascular degradation and is common in patients with repeated hospital admissions or patients admitted for prolonged periods of time.5. These patients are more likely to receive a central venous catherter, not because it is clinically necessary but because peripheral access was not secured.5 Studies show that ultrasound-guided peripheral IV catheter placement in DIVA patients is successful 76% to 100% of the time.6 Therefore recognizing DIVA patients early and using ultrasound guidance to insert peripheral IV catheters can reduce the number of failed insertion attempts and increase first stick success.3,6
When there is a delay in establishing vascular access, there is a delay in the administration of fluids and/or medication.4 In hospital departments such as Emergency or Intensive Care Units, this delay could negatively affect the patient's health. Recognizing DIVA patients early and using ultrasound guidance for peripheral IV insertions can significantly increase the success rates of peripheral IVs thereby improving patient care.3
The average time for peripheral IV insertion is reported from anywhere between 2.5 to 13 minutes.4 For DIVA patients, the insertion time could be as long as 30 mins.4 When a peripheral IV fails, every reinsertion attempt afterwards represents a signficant cost to the hospital and loss of productivity for the healthcare worker. Using ultrasound-guided peripheral IV insertion on the first attempt for DIVA patients can reduce hospital costs and give healthcare workers more time for patient care.3
DIVA patients are often escalated to central venous catherization to achieve vascular access, however this presents additional risks such as venous deep vein thrombosis, inadvertent arterial puncture, arterial cannulation, catheter associated infection, and pneumothorax.7 Ultrasound-guided peripheral IV insertions present a more desireable vascular access procedure for DIVA patients who are receiving a central line only because a peripheral IV insertion attempt failed.4
Although the insertion rate of ultrasound-guided peripheral IV catheters in patients with difficult vascular access is successful 76% to 100% of the time, the catheter dwell rate is concering, with 46% to 56% of the catheter failure occuring prematurely.6 According to a study that compared ultralong PIVCs to standard long PIVCs in peripheral ultrasound-guided insertions, catheter length in the vein is directly related to catheter longevity.6 Various studies have indicated that peripheral IV catheters have a higher survival rate when more than 65% of the catheter is in the vein.1,6 The longest standard length catheter on the market today is approximately 1.88 inches (4.78cm). This would mean that the ideal target vein should not be more than 2 cm from the skin surface.1,6
However with the ultralong peripheral IV catheter, Introcan Safety Deep Access, much deeper veins can be cannulated under ultrasound guidance. Introcan Safety Deep Access has catheters with a length of 2.5 inches (6.35 cm) in various gauges and a length of 1.25 inches (3.175 cm) in 24 gauge.
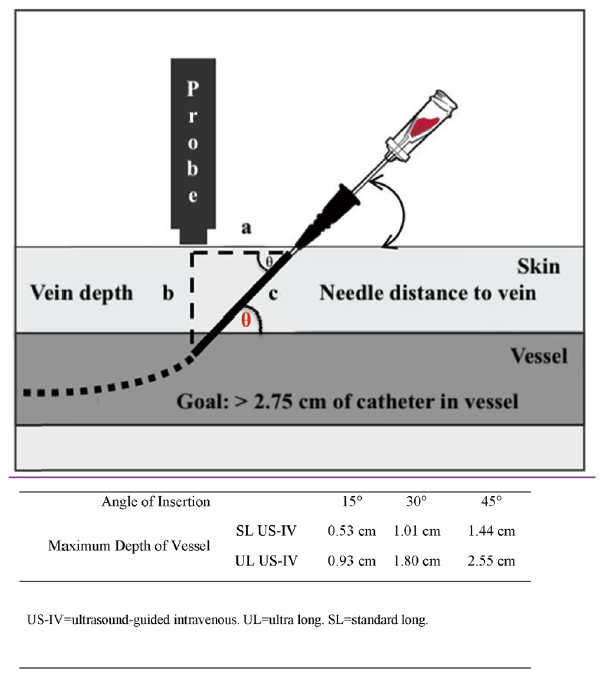 2.75 cm Rule. Bahl study recommendation on catheter length was based on depth of the vessel and inserter preference for the angle of insertion.
2.75 cm Rule. Bahl study recommendation on catheter length was based on depth of the vessel and inserter preference for the angle of insertion.
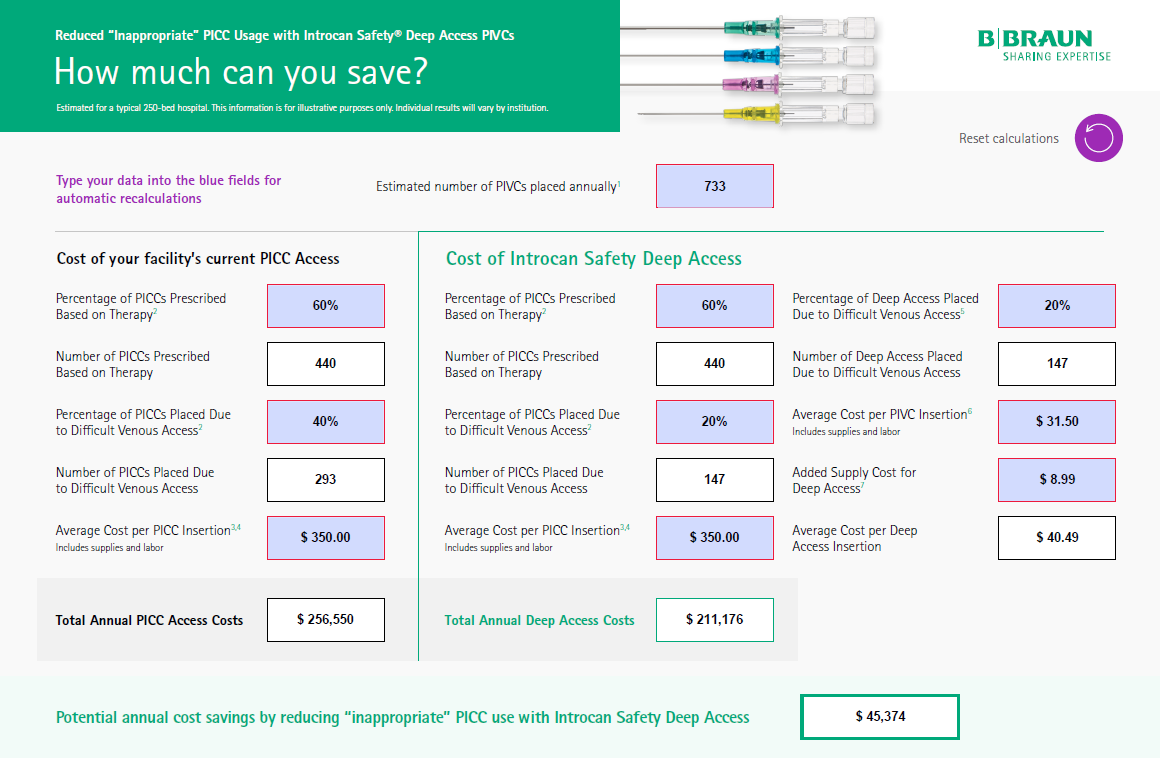
DIVA patients are likely to require the insertion of central lines not because of a therapeutic indication but rather due to difficulties securing a peripheral device.5
Speak with a B. Braun Strategic Account Manager to Assess Your Potential Savings with this Calculator
*Asterisk indicates required field
1. Blanco P. Ultrasound-guided peripheral venous cannulation in critically ill patients: a practical guideline. Ultrasound J. 2019 Oct 17;11(1):27. doi: 10.1186/s13089-019-0144-5. PMID: 31624927; PMCID: PMC6797689.
2. Helm, R. E. MD. et al. Accepted but Unacceptable: Peripheral IV Catheter Failure. The Art and Science of Infusion Nursing. (2015) https://doi.org/10.1097/NAN.0000000000000100
3. Van Loon FH, Van Hooff LW, de Boer HD, Koopman SS, Buise MP, Korsten HH, Bouwman AR. The modified A-DIVA scale as a predictive tool for prospective identification of adult patients at risk of a difficult intravenous access: A multicenter validation study. Journal of Clinical Medicine. 2019;8(2):144-156Whalen, M., Maliszewski, B. and Baptiste, D.L., 2017. Establishing a dedicated difficult vascular access team in the emergency department: a needs assessment. Journal of Infusion Nursing, 40(3), pp.149-154.
4. 2011 ENA Emergency Nursing Resources Development Committee; Crowley M, Brim C, Proehl J, Barnason S, Leviner S, Lindauer C, Naccarato M, Storer A, Williams J, Papa A. Emergency Nursing Resource: difficult intravenous access. J Emerg Nurs. 2012 Jul;38(4):335-43. doi: 10.1016/j.jen.2012.05.010. PMID: 22770395.
5. Rodríguez-Calero MA, Blanco-Mavillard I, Morales-Asencio JM, Fernández-Fernández I, Castro-Sánchez E, de Pedro-Gómez JE. Defining risk factors associated with difficult peripheral venous Cannulation: A systematic review and meta-analysis. Heart Lung. 2020 May-Jun;49(3):273-286. doi: 10.1016/j.hrtlng.2020.01.009. Epub 2020 Feb 11. PMID: 32057426.
6. Amit Bahl, MD, MPH; Mahmoud Hijazi, BA; Nai-Wei Chen, PhD; Ludovic Lachapelle-Clavette, BA; Jacob Price, MD. (2020). Ultralong Versus Standard Long Peripheral Intravenous Catheters: A Randomized Controlled Trial of Ultrasonographically Guided Catheter Survival. Ann Emerg Med. pii S0196-0644(19)31383-6. doi: 10.1016/j.annemergemed.2019.11.013.
7. Woodfall K, van Zundert A. Central Venous Access: An Update on Modern Techniques to Avoid Complications. Healthcare (Basel). 2025 May 16;13(10):1168. doi: 10.3390/healthcare13101168. PMID: 40428004; PMCID: PMC12111573.